Research
Cancer arises through an evolutionary process in which normal cells acquire mutations that erode growth controls, leading to the expansion of aberrantly proliferating cells. Such mutations activate cancer-promoting genes (oncogenes) or inactivate tumor suppressor genes, bestowing new capabilities to developing cancer cells. Our research is based on the premise that the path of cancer evolution dictates a tumor’s subsequent response to therapy and creates unique vulnerabilities that represent therapeutic opportunities.
Early work from our team identified p53 as an important regulator of apoptosis and cellular senescence and showed that apoptosis and senescence can act as a brake to oncogenic transformation in vitro and to tumorigenesis in vivo. In parallel, we showed that p53 could be a determinant of responses to conventional chemotherapy, providing one of the first indications that cancer genotype is intimately linked with therapy response. More recently, we have focused on detailed studies of p53 action and the consequences of p53 mutation, showing how p53 control of cell metabolism can influence cell state transition in cancer, and how the genomic instability that accompanies p53 loss leads to cancer genome evolution and more aggressive cancers.
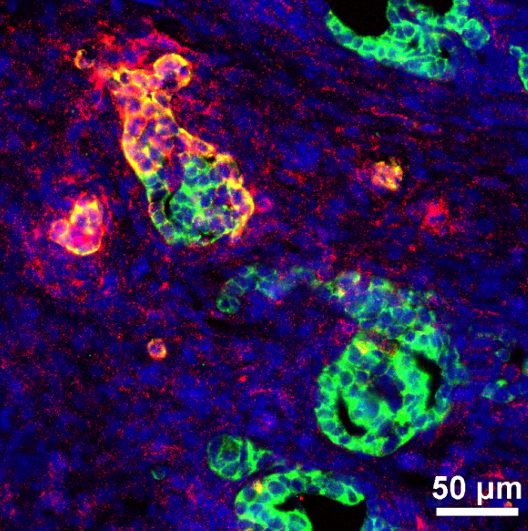
Figure 1
We are also interested in harnessing our knowledge of tumor suppressor biology to develop new therapeutic strategies. Some of these strategies arose from basic work showing that senescence induction can stimulate immune surveillance of senescent cells. Based on this, we are exploring therapeutic strategies that induce senescence in tumor cells as a means to enhance anti-tumor immunity. On the other hand, senescence surveillance mechanisms can fail, leading to the accumulation of senescent cells during chronic tissue damage pathologies and during aging. Based on work from others showing that, in these settings, senescent cells are deleterious, we are also developing innovative strategies to eliminate senescent cells from tissues with the goal of treating chronic tissue damage and age-related diseases.
Our approach combines the use of sophisticated mouse models, genetic tools, and genomic approaches to interrogate cancer phenotypes in a comprehensive way. More recently we have combined these tools with single-cell analytic approaches to study cell state and cell composition changes during tumor progression, as well as the interplay between cancer cells and the immune system in cancer therapy.
Current Projects:
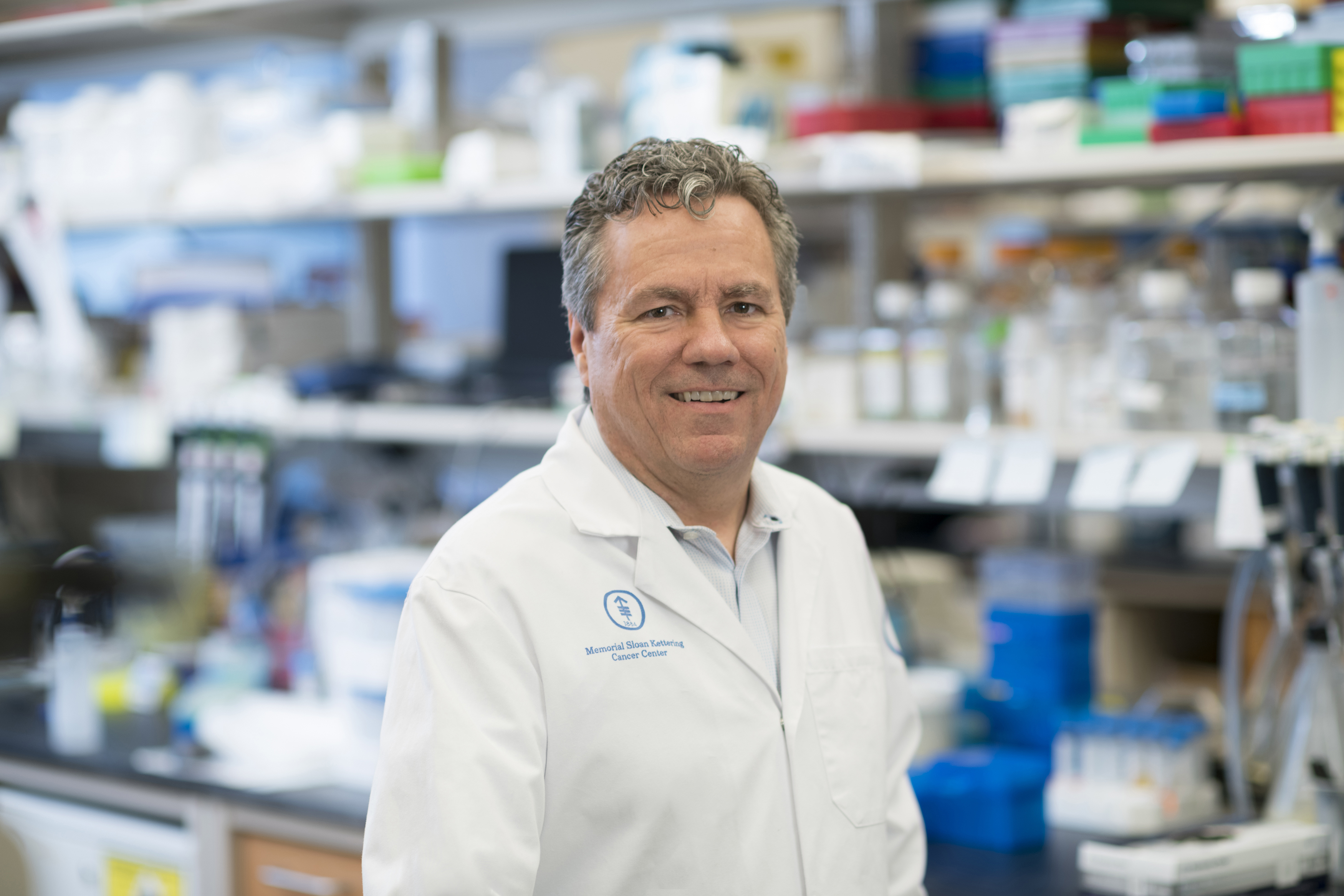
Bio
Scott W. Lowe is Chair of the Cancer Biology and Genetics Program at Memorial Sloan Kettering Cancer Center (MSKCC) in New York City and an Investigator for the Howard Hughes Medical Institute. Dr. Lowe received his bachelor’s degree from the University of Wisconsin-Madison and his Ph.D. from the Massachusetts Institute of Technology. He initiated his independent research at Cold Spring Harbor Laboratory, where his group made important contributions to our understanding of the p53 tumor suppressor network, as well as the processes of multi-step carcinogenesis, cellular senescence, and tumor-cell drug resistance. At MSKCC, his laboratory applies mouse models, functional genomics and cancer genomics in a coordinated effort to identify cancer drivers and dependencies. These efforts have revealed fundamental insights into cancer mechanisms and identified potential therapeutic targets.
Distinctions:
- HMI Investigator
- Elected member of the American Academy of Arts and Sciences, the National Academy of Science, and the National Academy of Medicine
- Fellow of the American Association of Cancer Research.
- Outstanding Investigator Award and G.H.A. Clowes Award from the American Association for Cancer Research
- Paul Marks Prize
- Alfred G. Knudsen Award from the NIH
