Research
Inflammatory bowel disease (IBD) affects over 2 million Americans. While advances in medical therapy have improved the care of IBD patients, many still suffer from refractory disease with significant morbidity. IBD includes two distinct clinical phenotypes called Crohn’s disease and ulcerative colitis. Although genetic polymorphisms correlate with disease susceptibility, environmental triggers including diet and intestinal bacteria are thought to play a central role in disease pathogenesis. While certain intestinal bacteria may act as opportunistic pathogens causing infection and inflammation, we and others have shown that microbiota function as a double-edged sword by simultaneously working to maintain homeostasis at mucosal surfaces. Thus, the major focus of our work is to define the cellular, molecular, and microbial regulation of intestinal barrier immunity and to develop novel diagnostic and therapeutic approaches for medically refractory IBD.
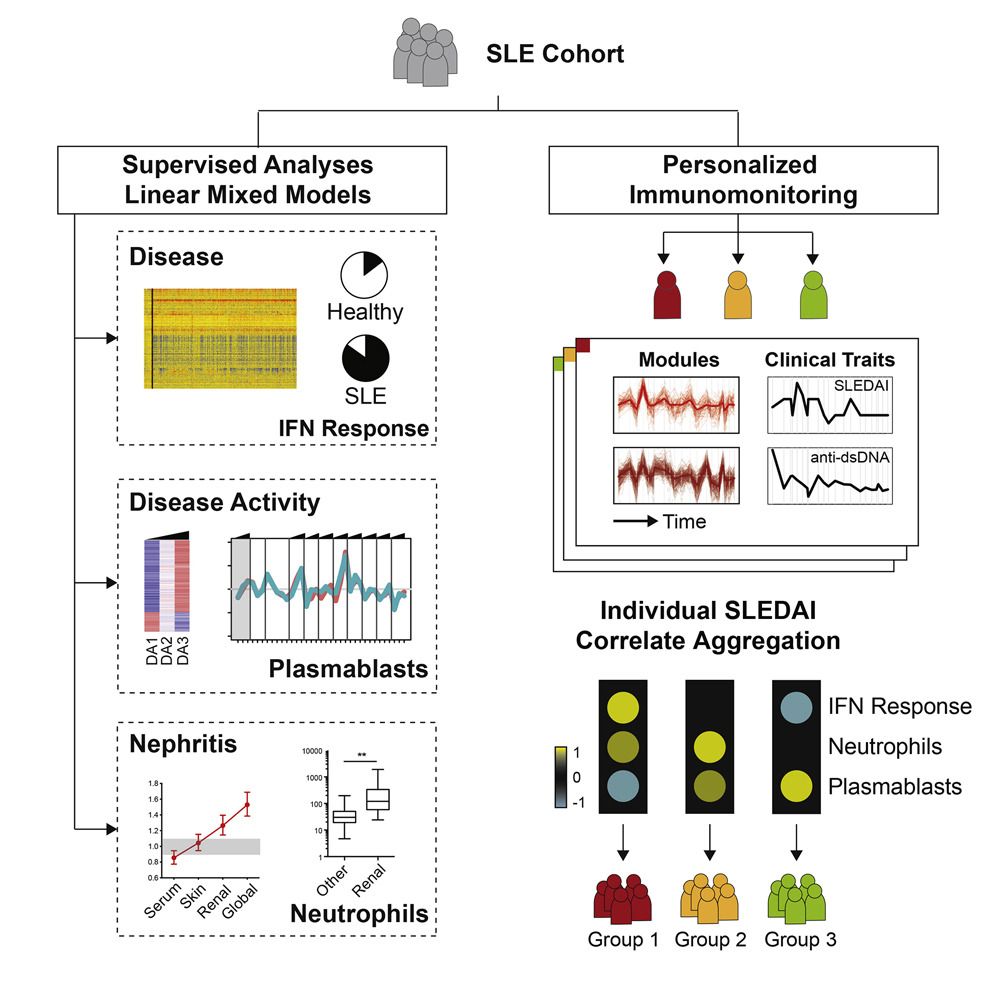
Figure 1.
Current Projects:
- Innate lymphoid cell biology
- Gut Microbiome
Bio
Randy Longman is the Director of the Jill Roberts Center for IBD and an Associate Professor of Medicine in the Jill Roberts Institute for Research in IBD at Weill Cornell Medicine. His research focuses on defining the cellular and molecular mechanisms underlying host-microbiota interactions that drive the pathogenesis of mucosal and systemic inflammation in IBD. He has received research funding from many foundations including the NIH and the Crohn’s and Colitis Foundation and is a member of the American Society for Clinical Investigation.
Distinctions.
- Elected member, ASCI.
