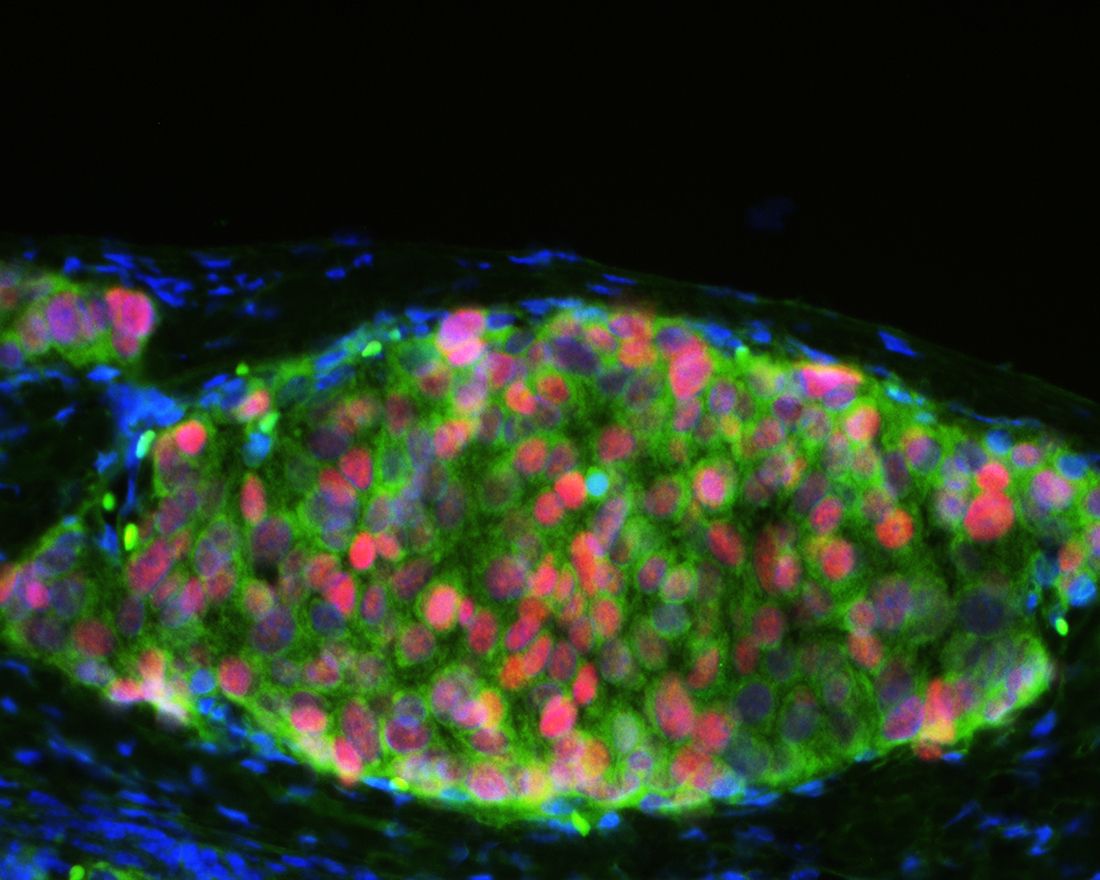
This image shows human embryonic stem cell-derived pancreatic beta cell clusters after being transplanted into immunodeficient mice. Image credit: Drs. Hui Zeng and Min Guo
An innovative method that uses human embryonic stem cells to model type 2 diabetes caused by genetic mutations may enable researchers to identify drugs that could treat the disease. The research by Weill Cornell Medicine investigators was published Aug. 11 in Cell Stem Cell, and may extend the use of precision medicine to metabolic diseases.
Using precision medicine approaches that target genetic mutations "is becoming commonly used in cancer, and we think it may be an approach we can use for diabetes," said senior study author Dr. Shuibing Chen, an assistant professor of chemical biology in surgery at Weill Cornell Medicine.
Type 2 diabetes is a condition in which the body does not correctly respond to insulin, a hormone that regulates the amount of glucose, or sugar, in the blood. As a result, people with the condition have high blood sugar levels. While obesity is a risk factor for diabetes, people may develop the disease for a variety of reasons. Genomic studies scanning complete sets of DNA have revealed many genetic mutations implicated in diabetes. But the precise role of these mutated genes, including three chosen for this study — CDKAL1, KCNQ1 and KCNJ11I — has been largely unknown.
To determine the functional role of these genetic mutations, Dr. Chen and colleagues, including Dr. Todd Evans, the Peter I. Pressman, M.D. Professor in Surgery at Weill Cornell Medicine, and Dr. Johannes Graumann, an assistant professor of biochemistry at Weill Cornell Medicine-Qatar, used human embryonic stem cells that were directed to function like pancreatic cells. The cells, called beta-like cells, produce, store and release insulin.
The investigators found that mutations in CDKAL1, KCNQ1 and KCNJ11I hinder the function of beta cells, resulting in decreased insulin release and problems with the regulation of blood sugar levels. They found the same to be true when the cells were studied in a Petri dish or when used in mouse studies. CDKAL1 mutations also caused the beta cells to be highly sensitive to high blood sugar and high fat levels, both of which are a common cause of beta cell death in diabetic patients.
The investigators then screened 2,000 drugs and found "one compound in phase II clinical trials that corrects the CDKAL1-related beta cell defect," Dr. Chen said. Dr. Chen and study co-authors Dr. Hui Zeng and Dr. Min Guo have filed a patent on the application of this compound for the treatment of CDKAL-related beta cell defects. Based on these study results, scientists may be able to "develop gene variant-specific therapy for different categories of diabetic patients," she said.
